If the thoracic aneurysm was caused by trauma, such as if the patient was in an accident, TEVAR is a way to rapidly cover and protect the injured area, controlling bleeding and preventing death.
Although surgical treatments for thoracic aortic aneurysms are available, surgery has a significantly higher risk of serious complications and death
How does it work?
In most cases, the patient is given an general anaesthetic or an epidural and a local anaesthetic for the procedure.
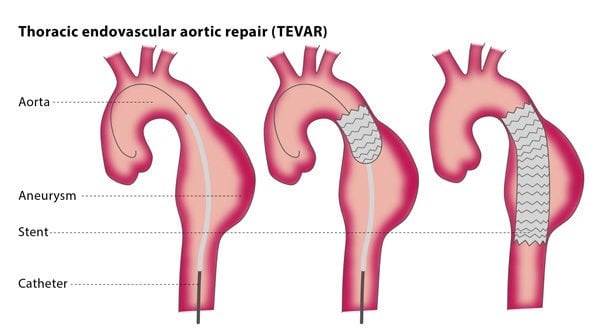
The interventional radiologist will make a small cut in an artery at the top of your legs and will insert a sheath (a short tube to maintain safe access to the vessels). Then, the interventional radiologist will insert guidewires and catheters (thin flexible tubes) and direct them to the affected area under fluoroscopy. A contrast medium (dye) will be injected into the thoracic aorta so that the area clearly shows up under imaging for maximum accuracy. To place the stent, the interventional radiologist will insert it over a guidewire and move it to the correct location, where it will expand to seal the aneurysm or cover any leaks in the wall of the vessel.
After the procedure, your vital signs will be monitored and you will stay in hospital for 2-3 days. You may experience bruising and pain, though this can be treated with standard painkillers. Moving around once you are able to do so is encouraged. You will need to have the stent regularly checked using CT or ultrasound to ensure that the stent is in good condition and to avoid long-term problems.
What are the risks?
The rate of successfully placing the stent and covering the aneurysm or tear is 98-99%. There are lower rates of pain and serious complications than with surgery, but the main risks associated with TEVAR are the stent displacement and blood collecting in the aneurysm again. This means that you will require regular monitoring, so that if any problems do occur, they can be resolved as soon as possible.
Minor complications include the risk of bruising and infection. There are some serious complications associated with the procedure, including death, stroke, tissue death, limb loss and injury to the kidneys. The rate of serious complications is estimated to be less than 15%, and the risk of death during the procedure is less than 1.5%.. There is also the possibility of the thoracic aorta tearing during the procedure, and in rare cases the spinal cord is injured, causing paralysis. Some patients react to the iodine in the dye used for imaging, which can affect the kidneys.
Bibliography
1. Aneurysmal disease: thoracic aorta. Hoel AW. Surg Clin North Am. 2013 Aug; 93(4):893-910, ix. doi: 10.1016/j.suc.2013.05.001
2. Endovascular stent-graft placement or open surgery for the treatment of acute type B aortic dissection: a meta-analysis. Zhang H, Wang ZW, Zhou Z, Hu XP, Wu HB, Guo Y. Ann Vasc Surg. 2012 May; 26(4):454-61. doi: 10.1016/j.avsg.2011.09.004.
3. Endovascular aortic repair versus open surgical repair for descending thoracic aortic disease a systematic review and meta-analysis of comparative studies. Cheng D, Martin J, Shennib H, Dunning J, Muneretto C, Schueler S, Von Segesser L, Sergeant P, Turina M. J Am Coll Cardiol. 2010 Mar 9; 55(10):986-1001. doi: 10.1016/j.jacc.2009.11.047. Review.
4. Thoracic Endovascular Aortic Repair (TEVAR) for the treatment of aortic diseases: a position statement from the European Association for Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Grabenwöger M, Alfonso F, Bachet J, Bonser R, Czerny M, Eggebrecht H, Evangelista A, Fattori R, Jakob H, Lönn L, Nienaber CA, Rocchi G, Rousseau H, Thompson M, Weigang E, Erbel R. Eur Heart J. 2012 Jul; 33(13):1558-63. doi: 10.1093/eurheartj/ehs074.