Why perform it?
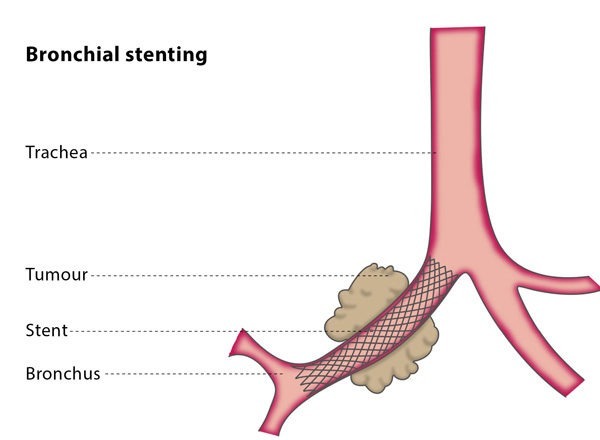
If you have a cancerous growth in your trachea or bronchi which cannot be operated on and is affecting your breathing, having a stent placed may relieve your breathlessness while you undergo chemotherapy and/or radiotherapy.
Stents can also be used to relieve symptoms from fistulas (a hole between two different compartments of the body which should not exist). A fistula may be due to cancer or surgery, endoscopy, or trauma. The stent is used to close this hole by covering it from one side so that no further leak occurs, and you can heal more quickly. In this case, the stent may be removed after the fistula is completely healed.
If the patient is a child, biodegradable stents which are absorbed over time are often used.
How does the procedure work?
You will have general anaesthetic for the procedure, which will be done in an operating theatre by a team of interventional radiologists and surgeons or pulmonologists. The doctors will use fluoroscopy and a bronchoscope (a tiny camera inserted into your body on a tube) for guidance.
An interventional radiologist will thread a guidewire (metallic wire) into your airway system so that the stent can be guided to the correct location. Once placed in the affected area, the stent will expand, clearing the airway. This procedure may be performed only on fluoroscopy (X-ray) guidance or along with bronchoscopy.
An interventional radiologist may take a tissue (biopsy) sample before the stent is placed.
In most cases, you will stay in the hospital overnight, sometimes longer, depending on how fast your symptoms disappear, and you will be discharged from the hospital once your pulmonologist, oncologist, or thoracic surgeon thinks it is safe.
What are the risks?
Most cases are successful, and most patients see significant improvement within 24-48 hours after the procedure. In 10-20% of cases, the stent migrates, meaning the stent can slip and move further down or get pushed up. If this occurs, the stent will be removed and replaced with a new stent.
Other possible complications include bleeding, chest infection, temporary chest pain (until the body gets used to the stent) and the risk of the airways reacting to the stents, which can cause spasms and breathlessness.
Post stenting, you may experience excess secretions from the respiratory system which may present as a cough with expectoration. This is your body reacting to an object in your windpipe. Please talk to your pulmonologist or the interventional radiologist or surgeon if you experience this and it bothers you greatly.
Bibliography
1. Inchingolo R, Sabharwal T, Spiliopoulos S, Krokidis M, Dourado R, Ahmed I, King J, Adam A. Tracheobronchial stenting for malignant airway disease: long-term outcomes from a single-center study. Am J Hosp Palliat Care. 2013 Nov; 30(7):683-9. doi: 10.1177/1049909112462861.
2. Du Rand IA, Barber PV, Goldring J, Lewis RA, Mandal S, Munavvar M, Rintoul RC, Shah PL, Singh S, Slade MG, Woolley A; BTS Interventional Bronchoscopy Guideline Group. Summary of the British Thoracic Society guidelines for advanced diagnostic and therapeutic flexible bronchoscopy in adults. Thorax. 2011 Nov; 66(11):1014-5. doi: 10.1136/thoraxjnl-2011-201052.
3. Katsanos K, Ahmad F, Dourado R, Sabharwal T, Adam A. Interventional radiology in the elderly. Clin Interv Aging. 2009; 4:1-15. Epub 2009 May 14. Review.