How does the procedure work?
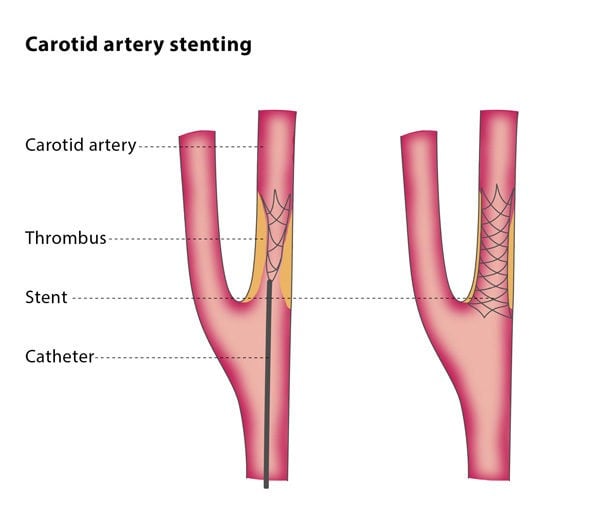
You will be given a local anaesthetic for the procedure. Using fluoroscopy to monitor and guide the process, the interventional radiologist will puncture an artery in your groin or arm with a needle, and will insert a balloon-tipped catheter into the carotid artery, guiding the catheter into the narrowed area. The balloon will then be inflated and deflated, compressing the fatty plaque or blockage against the artery walls, widening the blood vessel and increasing blood flow. After this, the balloon will be removed.
The interventional radiologist will use another catheter to place a stent, and, in some cases, will further expand the stent using another balloon-tipped catheter. The stent remains in place so that there is a clear passage in your artery.
Why perform it?
CAS may be an appropriate treatment for you if you have symptoms of carotid artery disease and are at increased risk of suffering complications from surgery. It may be beneficial if you have undergone traditional surgery but your arteries have become re-narrowed (called restenosis), if the location of the narrowing in the artery means it cannot be operated on or if narrowing has occurred following radiation treatment. It may also be considered as a treatment for you if you have no symptoms of carotid artery disease but are awaiting surgery for carotid stenosis.
What are the risks?
The most severe risks of CAS are stroke and death. Stroke can occur during the procedure and is usually caused by fragments dislodging from the plaque into the circulation of blood in the brain.
The minimally invasive treatment of CAS and the surgical treatment CEA have been shown to have similar short-term and long-term outcomes, though CAS is associated with a higher risk of stroke or death during the procedure if the patient is elderly. However, CAS has a lower risk of heart attack, cranial nerve palsy and bruising at the access site than CEA.
In some cases, patients experience a temporarily decreased heart rate or cardiac arrest when the carotid artery is widened at its main branch point, though these complications can be avoided when patients are given atropine.
Other possible complications of carotid artery stenting include spasm, the formation of blood clots, tearing in the artery wall and hyperperfusion syndrome, which can lead to problems with the nervous system.
You may also experience complications at the access site, including bleeding, bruising, blood clots, injury to the artery causing blood to leak and pool outside the arterial wall (called a pseudoaneurysm) and bleeding in the muscle and tissues behind the abdominal wall cavity. Many of these complications can be treated without surgery. You may have low blood pressure 2-24 hours after the procedure, but this does not cause any clinical problems.
Although it is uncommon, it is possible to have an allergic reaction to the dye used to enhance imaging.
Bibliography
1. Bonati LH, Lyrer P, Ederle J, Featherstone R, Brown MM. Percutaneous transluminal balloon angioplasty and stenting for carotid artery stenosis. Cochrane Database Syst Rev. 2012 Sep 12.
2. Brott TG et al, Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis. N Engl J Med 2010; 363:11-23.