Why perform it?
If you have large tumours in your liver, kidneys, lungs or bones, this treatment may be beneficial for you. There are different ways in which embolization can be used in oncology. It can be used simply to cut off blood supply to the tumour (bland embolization), or combined with chemotherapy to deliver the drugs directly into the tumour (chemoembolization), or the particles may contain doses of radiation to selectively kill the tumour cells (radioembolization).
Embolization is also suitable for some non-cancerous tumours. Occasionally, embolization may be used to reduce blood supply before a surgical removal of a tumour to reduce blood loss during operation.
How does the procedure work?
You should not eat anything before the procedure, and you may be given a sedative to help you relax. It is important that you stay still during the procedure to ensure that the X-ray images taken are accurate. The procedure will last around one hour.
You will be given a local anaesthetic for the procedure. The interventional radiologist will puncture an artery in your thigh with a small needle and will then thread a combination of plastic tubes (called sheaths and catheters) and guidewires into your arteries.
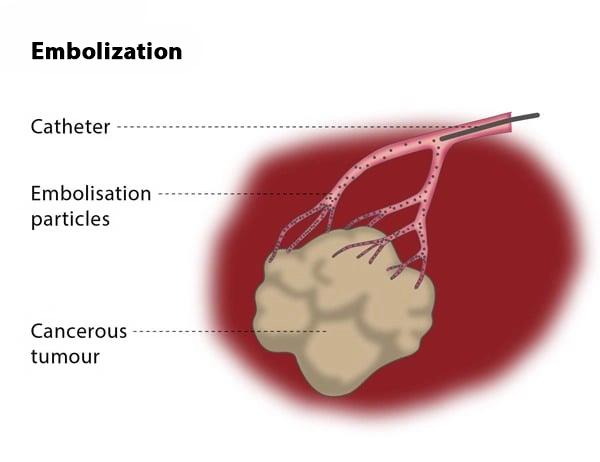
The interventional radiologist will inject a contrast medium (dye) through a catheter so that the area can be seen clearly under imaging. Then, the interventional radiologist will carefully navigate a microcatheter as close as possible to the tumour and will release the embolic particles. The particles are usually microspheres that are less than 0.5 mm in size, and these may be combined or loaded with chemotherapy or radiations emitting substances such as yttrium 90.
Most patients experience some pain and nausea after the procedure, so you will be offered strong painkillers and medication to prevent nausea. You may be discharged on the same day, but if you experience severe symptoms after the procedure you may need to stay in hospital overnight.
What are the risks?
The technical success rate, defined as successful delivery of the particles into the tumour, is usually over 95%. Clinical success (defined as a partial or complete death of the tumour and shrinkage of the tumour) and is around 30-50%, though it varies depending on the location, extent and biology of the underlying disease.
You may be offered multiple treatments to optimise the response, and 10-20% of the cases may also require further treatment (surgery or ablation) in the future.
The main risk is non-target embolization, meaning that the particles are accidentally released to normal vessels, which may destroy healthy tissue or restrict blood supply to an organ. Less severe side effects include bleeding, bruising and infection at the puncture site. In rare cases, the patient experiences abdominal haemorrhage, meaning they must stay in hospital and may need blood transfusions.
It is possible to have an allergic reaction to the contrast medium or for the iodine in the dye to affect the kidney. There is also a risk of post-embolization syndrome, which causes fever, nausea and pain.
Bibliography
1. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. European Association for Study of Liver; European Organisation for Research and Treatment of Cancer. Eur J Cancer. 2012 Mar; 48(5):599-641. doi: 10.1016/j.ejca.2011.12.021.
2. Chapiro J, Tacher V, Geschwind JF. Intraarterial therapies for primary liver cancer: state of the art. Expert Rev Anticancer Ther. 2013 Oct; 13(10):1157-67. doi: 10.1586/14737140.2013.845528
3. Mahnken AH, Spreafico C, Maleux G, Helmberger T, Jakobs TF. Standards of practice in transarterial radioembolization. Cardiovasc Intervent Radiol. 2013 Jun; 36(3):613-22. doi: 10.1007/s00270-013-0600-8.