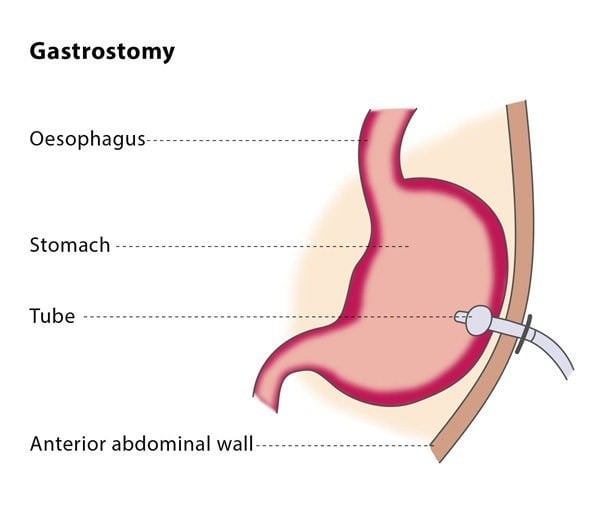
The position of the needle tip within the stomach is confirmed using air or contrast media under imaging. The interventional radiologist will then position a guidewire through the needle and into your stomach, followed by a series of dilators which will be inserted over the guidewire to expand the area around it. The gastrostomy tube will then be inserted into your stomach. It has a balloon at the end which will be inflated to keep it in place and the guidewire will be safely removed. The interventional radiologist will inject a few millilitres of contrast media through the gastrostomy tube so that the position of the tube can be checked using fluoroscopy.
You will probably be asked to stay in hospital overnight, though the procedure can in some cases be performed as an out-patient procedure. You may experience some discomfort around the catheter in the first few hours following the procedure.
The entry point for the gastrostomy tube should be checked daily for signs of leakage or infection. You will be able to begin eating again few hours after the procedure. The gastropexy anchors can be safely removed 10-14 days after the procedure.
The technical success rate of the gastrostomy procedure is very high, at around 97%.
Why perform it?
As a general rule, enteral feeding (delivering food directly into the stomach) is recommended when a patient is unable to eat for at least 7-14 days. If you have been unable to eat normally for more than 30 days, you may be recommended to have a gastrostomy or a gastrojejunostomy tube placed.
The most common reasons for being unable to eat are neurological causes that prevent normal swallowing (such as stroke or dementia), anatomical situations (such as during correction procedures of cleft lip and palate anomalies) and obstruction of the gullet (such as presence of head and neck tumours, post-radiation conditions). If you have a cancerous tumour in your bowel which causes a blockage, you may be recommended for a gastrostomy tube to decompress the stomach.
What are the risks?
The most common complications include skin infection around the gastrostomy entry point and bruising. It is possible that the colon could be perforated during the placement of the tube, which can lead to severe peritonitis. If the gastrostomy tube is placed through the left hepatic lobe of your liver, you may experience bruising in your liver.
As long as you are suitable for the procedure and the interventional radiologist chooses the technique most suited for you, the risk of complications is low (the rate of major complications is less than 3%).
Bibliography
1. de Baere T, Chapot R, Kuoch V, et al. Percutaneous gastrostomy with fluoroscopic guidance: a single-centre experience in 500 consecutive cancer patients. Radiology 1999; 210(3):1076-83.
2. Covarrubias DA, O’Connor OJ, McDermott S, Arellano RS. Radiologic percutaneous gastrostomy: review of potential complications and approach to managing the unexpected outcome. AJR Am J Roentgenol 2013; 200(4):921-31.
3. Laasch HU, Martin DF. Radiologic gastrostomy. Endoscopy 2007; 39(3):247-55.
4. Given MF, Hanson JJ, Lee MJ. Interventional radiology techniques for provision of enteral feeding. Cardiovasc Intervent Radiol 2005; 28(6):692-703.