Patient selection is key, however, and not all patients are eligible for stenting reconstruction, for instance. Patient non-compliance to medication is one of the main reasons for stent occlusion, assuming technical success with good inflow and outflow.
I got the chance to see and scrub in for a few endovascular procedures in the setting of acute on chronic and chronic iliofemoral deep venous thrombosis, inferior vena cava reconstruction, and cava and/or iliofemoral stent recanalization after thrombosis. I operated and learned about unreplaceable IVUS, as well as different thrombectomy devices – angiojet, lightning and clotriever systems – and their best indications. I also learned which catheters and guidewires will help you along the way for specific situations.
There were also some cases of superficial venous disease treated by means of radiofrequency ablation of an incompetent great saphenous vein, phlebectomy, and foam sclerotherapy. I was able to watch a couple of cases of pelvic congestion syndrome treated using percutaneous treatment of vulvar varices, and a few cases of upper limb DVT treated by catheter-directed thrombolysis alone, and SVC syndrome treatment by angioplasty and stenting.
Furthermore, I got the chance to update my skills and learn tricks and tips on some procedures I don’t usually perform in my daily practice, such as uterine embolization, superior hypogastric nerve block, long standing IVC filters difficult removals, positioning of a double J ureteric stent, adrenal venous sampling, PICC lines, port-a-caths and permcaths.
I found the hospital setting at Galway University Hospital to be quite welcoming, and easy-going; obviously, the fact that there were almost no language barriers helped a lot. (But let’s just say, with all due respect, that the Irish accent can be a challenge for the first weeks!)
I became more aware of the set up needed to run a “venous clinic” and all the hard work involved in the process, before, during, and after endovascular treatment. Prof. Gerard O’ Sullivan is a great example to learn from and an outstanding teacher. I appreciated him and his team having me there very much
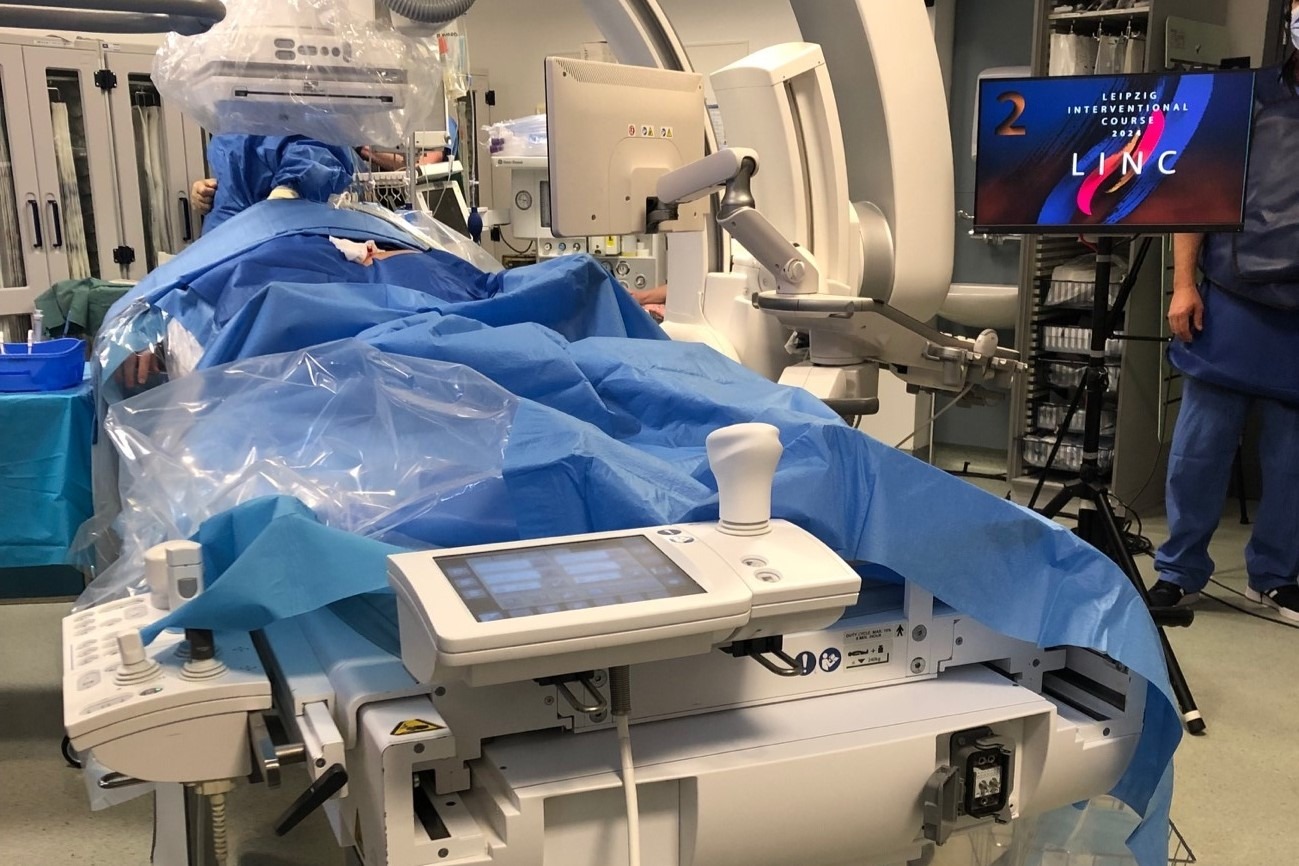
The cherry on top of the cake was being able to come back a few weeks later to help and take part in LINC’s venous cases live broadcasting!
My message to other IRs considering doing a fellowship, whether they are trainees, fellows or consultants is: Go for it! It is a challenging and refreshing experience where you can learn so much more than you initially set out to learn.
I am thankful to CIRSE to promote this great experience!