This fellowship allowed me to learn and participate in many procedures in different areas of IR, and I would point out the following areas and highlights:
Pain management is an essential skill set for all IRs, and the team in Athens does excellent work in carrying out these procedures. I was able to witness (among others):
- Cryoneurolysis (celiac plexus, splanchnic nerves…) in the context of intractable cancer pain (mostly pancreatic cancer);
- Cryoneurolysis of medial branch nerves for facet joint pain;
- Vertebroplasty/vertebral augmentation;
- Discectomy/disc decompression techniques;
- Infiltrations (epidural, nerve roots, facet joints, sacroiliac joints…);
- Pulsed radiofrequency nerve ablation.
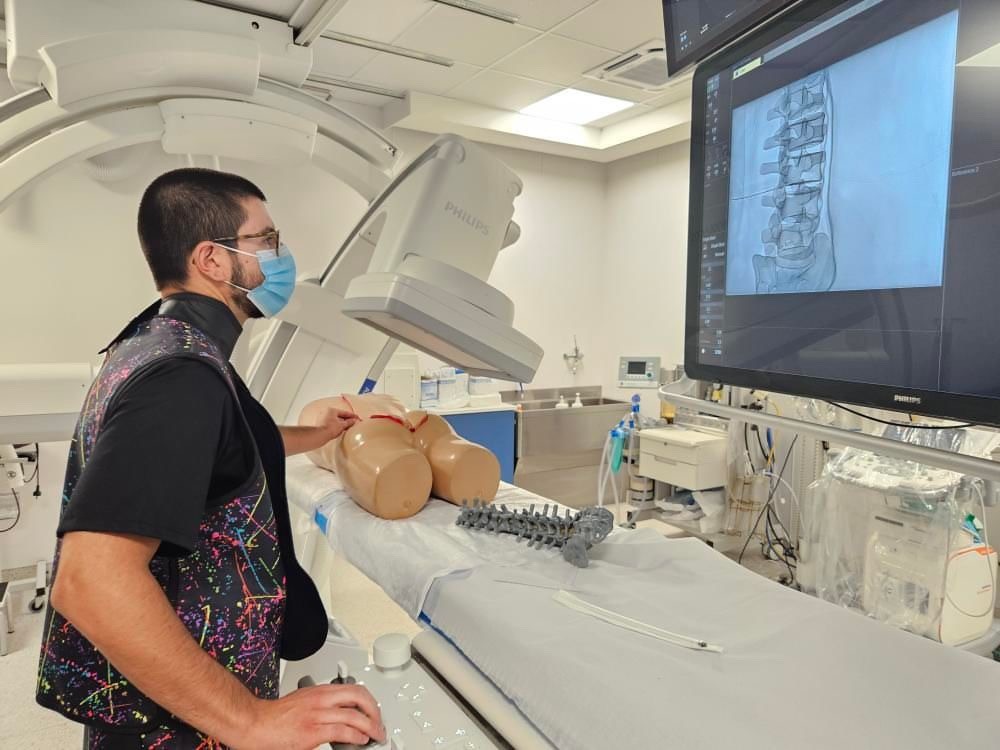
I also had the chance to improve my knowledge and skills in the area of pain management as well as other spine and musculoskeletal procedures, during the European School of IR (ESIR) course, “Spine interventions: Established indications”, with local host Prof. Dimitris Filippiadis. Fortunately for me, this course was held in “Attikon” Hospital during my stay. It was a successful event with great lectures and amazing hands-on workshops, allowing participants to explore techniques like epidural injections, facet joint and sacro-iliac joint therapies, intervertebral disc techniques, percutaneous bone biopsies, vertebroplasty, vertebral balloon augmentation, ultrasound-guided spine injections, and navigation systems (electromagnetic, robotic, combined endoscopy).
The team has published many papers on the topic of cancer pain management, including a publication (with Prof. Dimitris Filippiadis and Prof. Alexis Kelekis as authors) that was incorporated in the National Comprehensive Cancer Network (NCCN) 2021 guidelines for adult cancer pain. The impact of pain management through IR procedures and importance of ablation in cancer pain relief are evident here, whether it be percutaneous ablation on nerve structures responsible for pain mediation signals (neurolysis), or direct tumour ablation to relieve tumour-mediated inflammation and decompress tumour compression of anatomical structures.
Regarding other IO procedures, I was able to attend multiple transarterial radioembolization (TARE) and transarterial chemoembolization (TACE) procedures for the treatment of liver tumours (including hepatocarcinoma and cholangiocarcinoma).
Also, the team expertly performs numerous CT-guided ablation procedures (with different technologies, and in different organs,) including:
- Liver microwave (MW) ablation (mainly for colorectal cancer liver metastases);
- Lung metastases cryoablation;
- Renal cell carcinoma (RCC) cryoablation;
- Extra-abdominal desmoid tumour cryoablation.
It was a great experience watching the pre-procedural image assessment, planning, execution, and often follow-up of these embolization and ablation procedures.
I also had the chance to watch how adjunctive techniques can be applied to improve the efficacy and safety of ablation procedures, namely, transarterial embolization to decrease the vascularity of renal tumours before performing renal cryoablation, as well as planning thermal protective techniques (hydrodissection) to protect important anatomical structures.